What You Need to Know
- Testing is critically important to help reduce the spread of COVID-19.
- COVID-19 self-tests can be taken at home or anywhere, are easy to use, and produce rapid results.
- Self-tests (also referred to as at-home tests or over-the-counter (OTC) tests) are one of many risk-reduction measures, along with vaccination, masking, and physical distancing, that protect you and others by reducing the chances of spreading COVID-19.
- Free self-tests can be ordered at COVIDtests.gov.
- You can use COVID-19 self-tests regardless of vaccination status or whether or not you have symptoms.
- Consider using a COVID-19 self-test before joining indoor gatherings with others who are not in your household. This is especially important before gathering with individuals at risk of severe disease, older individuals, those who are immunocompromised, or unvaccinated people, including children who cannot get vaccinated yet.
- To obtain accurate results, follow all of the manufacturer’s instructions for performing the self-test.
- If you test positive, you should isolate and wear a well-fitting mask if you must be around others, inform your healthcare provider, and inform any close contacts. If you are a healthcare provider, follow CDC guidance for healthcare providers.
- A negative self-test result means that the test did not detect the virus that causes but it does not rule out a COVID-19 infection. A single negative self-test result may not reliable, especially if you have symptoms associated with COVID-19.
- If your result is negative, repeating the self-test within a few days, with at least 24 hours between tests, will increase the confidence that you are not infected with the virus causing COVID-19.
What is a Self-Test?
Self-tests for COVID-19 are those that can be performed on yourself at home or anywhere. Sometimes a self-test is also called a “home test,” an “at-home test,” or an “over-the-counter (OTC) test.” Self-testing offers fast results. Self-tests are one of several options for testing for the virus that causes COVID-19 and may be more convenient than laboratory-based tests and point-of-care tests.
Visit FDA’s website for a list of authorized tests. Some self-tests may have age limitations for self-collection or collection by an adult for a child.
As of January 2022, self-tests are used to detect current infection. No self-tests are available to detect antibodies to the virus, which would suggest previous infection.
When to Consider Self-Testing
Self-tests may be used if you have COVID-19 symptoms or have been in close contact or potentially in close contact with an individual with COVID-19.
Even if you don’t have symptoms and have not been in close contact with an individual with COVID-19, using a self-test before gathering indoors with others can give you information about the risk of spreading COVID-19. This is especially important before gathering with individuals at risk of severe disease, older individuals, those who are immunocompromised, or unvaccinated people, including children who cannot get vaccinated yet.
Specifically, the best timing when using a self-test is:
- If you have COVID-19 symptoms, use a self-test immediately
- If you were a close contact of someone with COVID-19, self-test after at least 5 days, plus a second test in 1 or 2 days if your first test is negative (See Serial Testing, below)
- If you are testing before a gathering, test immediately before the gathering (or as close in time to the event as possible)
How to Get a Self-Test
Self-tests can be purchased online or in pharmacies and retail stores. Private health insurance will reimburse the cost of purchasing self-tests.
Self-tests can be purchased online or in pharmacies and retail stores. They are also available at no cost through some local health departments, Federally Qualified Health Centers (FQHC), or by ordering at COVIDtests.gov
For a list of authorized self-tests, see FDA EUA Testsexternal icon. Some tests may have age limitations for self-collection or collection by an adult for a child. If you are unable to obtain a self-test, but have symptoms of COVID-19 or have been exposed, stay away from others as much as possible and follow CDC recommendations for What to Do If You Are Sick. You may also consider visiting a community testing site. Call your local health department for additional testing options.
How to Use a Self-Test
Read the complete manufacturer’s instructions for use before using the test. Talk to a healthcare provider if you have questions about the test or your results.
Prepare to Collect a Specimen
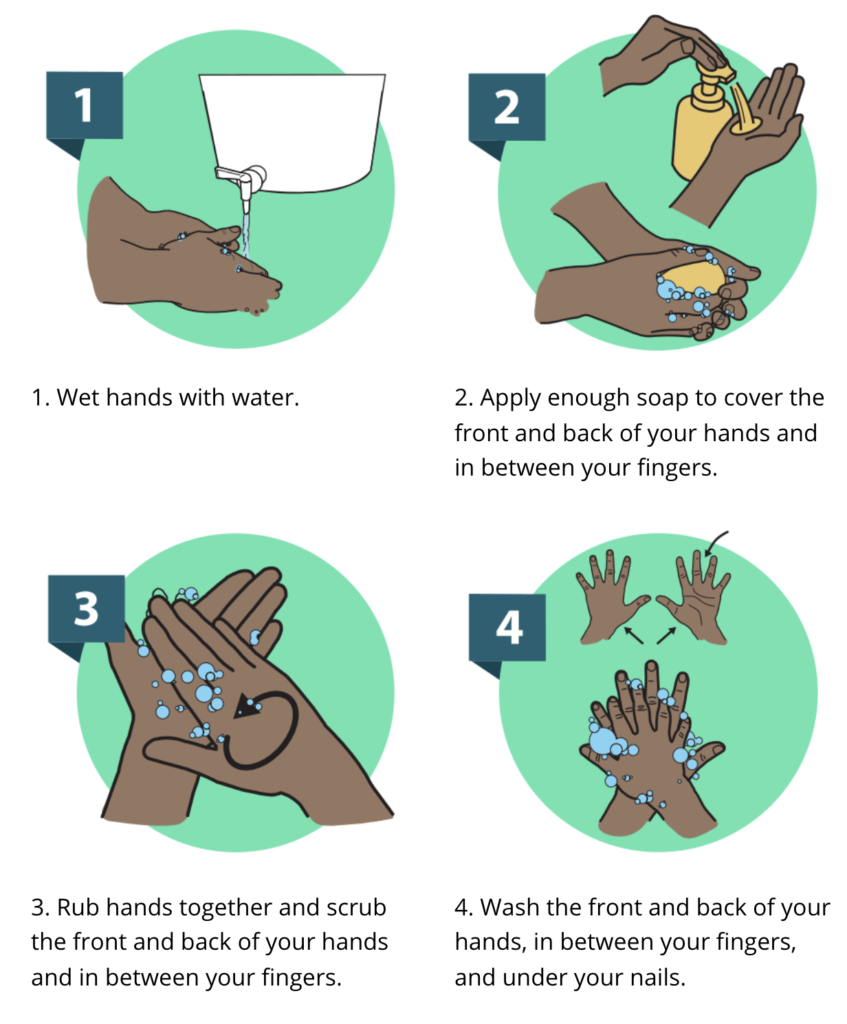
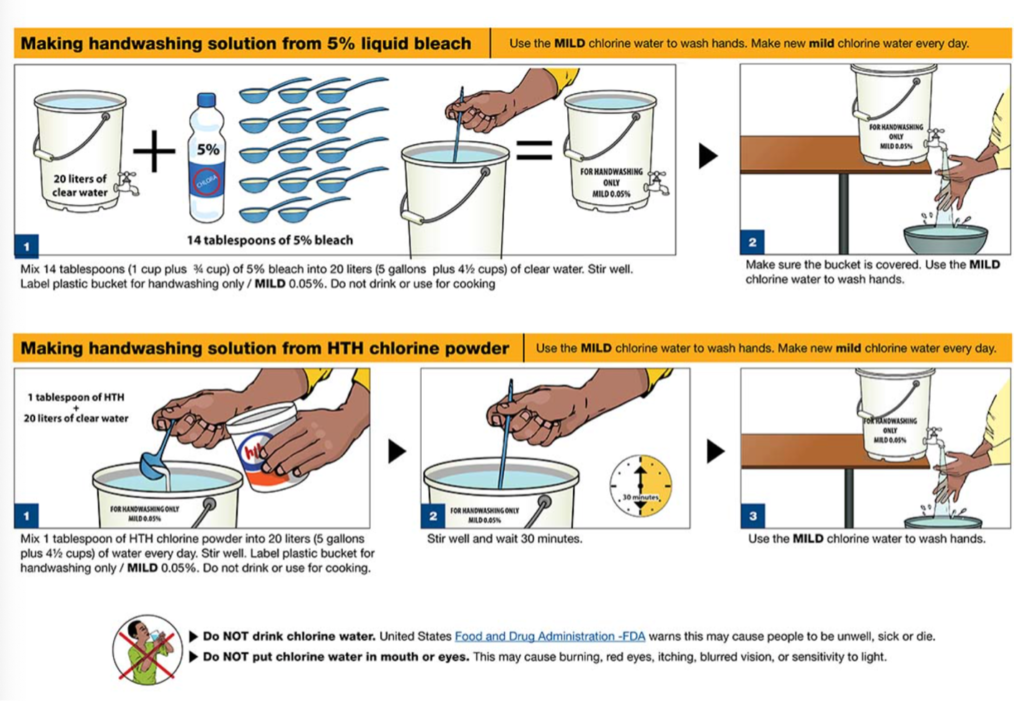
- Wash your hands with soap and water for at least 20 seconds.
- Open the box and follow the instructions included with the COVID-19 self-test to collect your own nasal specimen.
- If you do not collect the specimens as directed, your test results may be incorrect.
Collect a Specimen and Perform the Self-Test
Follow the manufacturer’s instructions exactly and perform the steps in the order that they are listed. The manufacturer may also provide other resources, such as quick reference guides or instructional videos, to help you perform the test correctly.
Most COVID-19 self-tests require the collection of a nasal specimen (see the Additional Print Resources section below).
Once collected, use the specimen as described in the instructions to complete the self-test.
If Your Test Result is Positive
You should isolate according to CDC recommendations and wear a well-fitting mask if you must be around other people. Report your positive result to your healthcare provider. It is particularly important to seek medical care and possible treatment if you have an underlying medical condition that increases your risks from COVID-19. If your illness becomes severe, seek medical attention. If you have an emergency warning sign (including trouble breathing), seek emergency medical care immediately. To avoid spreading the virus to others, follow CDC recommendations.
Tell your close contacts that they may have been exposed to the virus that causes COVID-19. A person with COVID-19 can begin spreading the virus starting 48 hours (or 2 days) before they have any symptoms or test positive. By informing your close contacts that they may have been exposed, you are helping to protect everyone.
If you think your positive test result may be incorrect, contact a healthcare provider to determine whether additional testing is necessary.
If Your Test Result is Negative
A negative test result means that the virus that causes COVID-19 was not detected in your specimen, and you may have a lower risk of transmitting the disease to others. If you took the test while you had symptoms and followed all instructions carefully, a negative result means your current illness may not be COVID-19, though it does not rule out COVID-19 infection.
It is also possible for a test to give a negative result in some people who have COVID-19. This is called a false negative. You could also test negative if the specimen was collected too early in your infection. In this case, you could test positive later during your illness. You should consider serial testing (see below).
Even if you receive a negative result, you should continue to practice preventative measures, such as being up to date on your COVID-19 vaccination, wearing a mask indoors, and physical distancing to reduce the risk of spreading COVID-19.
If Your Result Shows Invalid or Error
Sometimes invalid results or an error can occur on the self-test device. Invalid results or an error can occur for many reasons. Your specimen may not have been collected correctly, or the test may have malfunctioned.
Invalid test results are rare but can occur. If the self-test shows an invalid result or a test error, the test did not work properly. If this happens, a new test is needed to get an accurate result. Refer to the manufacturer’s instructions in the package insert and contact the manufacturer for assistance, consider taking another self-test, or contact a healthcare provider for additional help.
Serial Testing (Repeat Testing)
Serial testing is when a person tests multiple times for COVID-19, or on a routine basis, such as every few days. Some self-tests are designed to be used in a series. By testing more frequently, you may be able to detect COVID-19 more quickly and could reduce the spread of infection. Some self-tests include instructions for performing serial testing, including the number of days between tests, and may include more than one test in the package.
If your self-test is negative, you should follow the manufacturer’s instructions for serial testing, if applicable. Manufacturer’s instructions are included in the test box and are also available on the FDA website. The instructions may recommend you test again within 2 or 3 days. Contact a healthcare provider if you have any questions about your test results or serial testing. You may also use the COVID-19 Viral Testing Tool to help you determine the next steps after testing.
If you think your negative test result may be incorrect, contact a healthcare provider to determine whether additional testing is necessary.
To learn more, please visit https://www.cdc.gov/coronavirus/2019-ncov/testing/self-testing.html