MISCONCEPTIONS ABOUT FLU VACCINES
Can a flu vaccine give you flu?
No, flu vaccines cannot cause flu illness. Flu vaccines given with a needle (i.e., flu shots) are made with either inactivated (killed) viruses, or with only a single protein from the flu virus. The nasal spray vaccine contains live viruses that are attenuated (weakened) so that they will not cause illness.
Are any of the available flu vaccines recommended over the others?
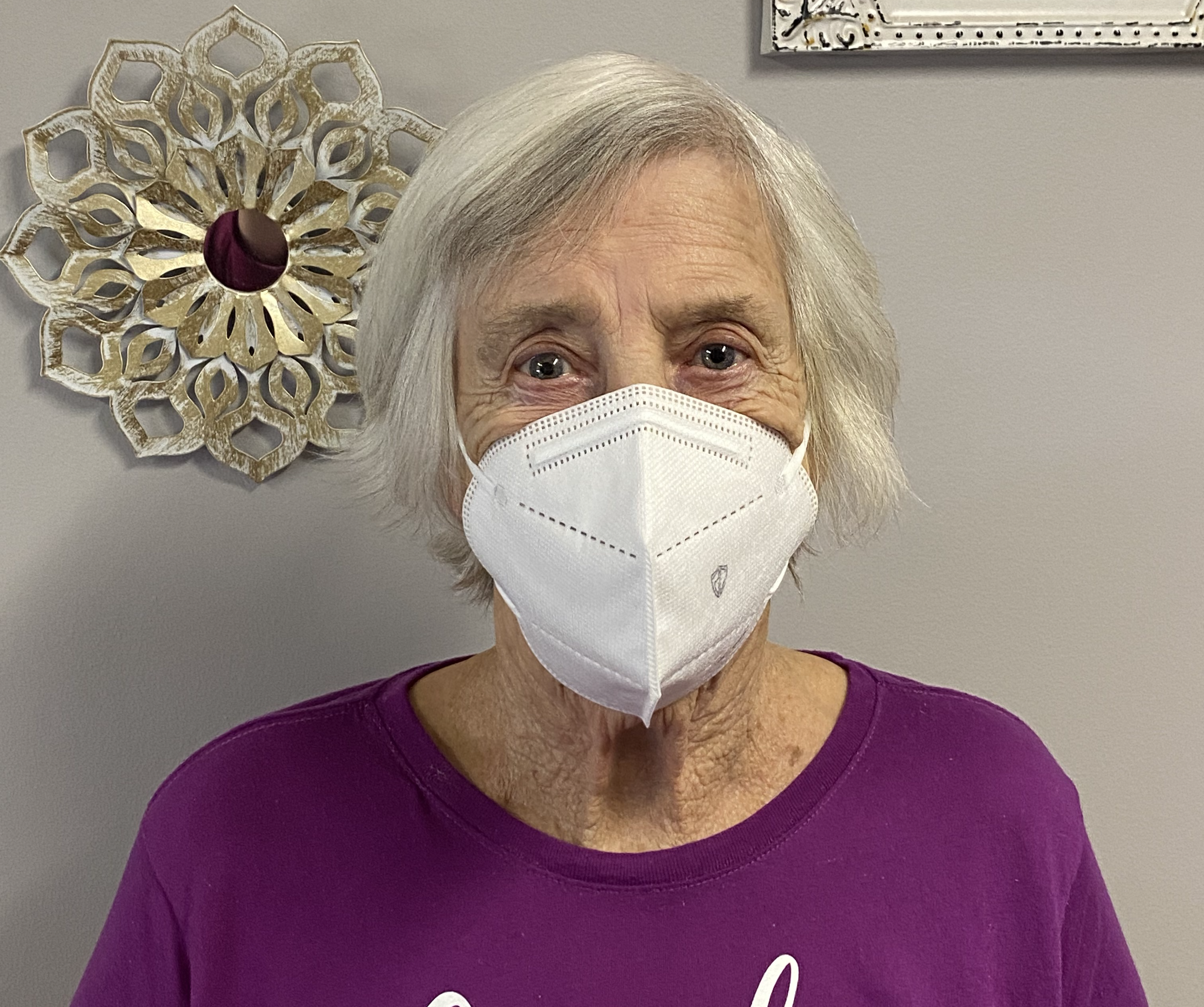
Yes, for some people. For the 2022-2023 flu season, there are three flu vaccines that are preferentially recommended for people 65 years and older. These are Fluzone High-Dose Quadrivalent vaccine, Flublok Quadrivalent recombinant flu vaccine and Fluad Quadrivalent adjuvanted flu vaccine. This recommendation was based on a review of available studies which suggests that, in this age group, these vaccines are potentially more effective than standard dose unadjuvanted flu vaccines. There is no preferential recommendation for people younger than 65 years.
What if a preferentially recommended flu vaccine is not available?
If none of the three flu vaccines preferentially recommended for people 65 years and older is available at the time of administration, people in this age group should get any other age-appropriate flu vaccine instead.
Is it better to get sick with flu than to get a flu vaccine?
No. Flu can be a serious disease, particularly among young children, older adults, and people with certain chronic health conditions, such as asthma, heart disease or diabetes. Any flu infection can carry a risk of serious complications, hospitalization or death, even among otherwise healthy children and adults. Therefore, getting vaccinated is a safer choice than risking illness to obtain immune protection.
Do I really need a flu vaccine every year?
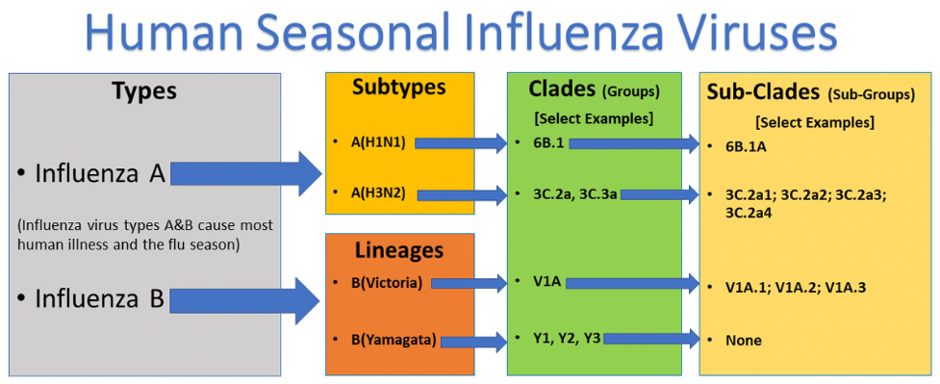
Yes. CDC recommends a yearly flu vaccine for everyone 6 months of age and older with rare exception. The reason for this is that a person’s immune protection from vaccination declines over time, so an annual vaccination is needed to get the “optimal” or best protection against the flu. Additionally, flu viruses are constantly changing, so the vaccine composition is reviewed each year and updated as needed.
Why do some people not feel well after getting a seasonal flu vaccine?
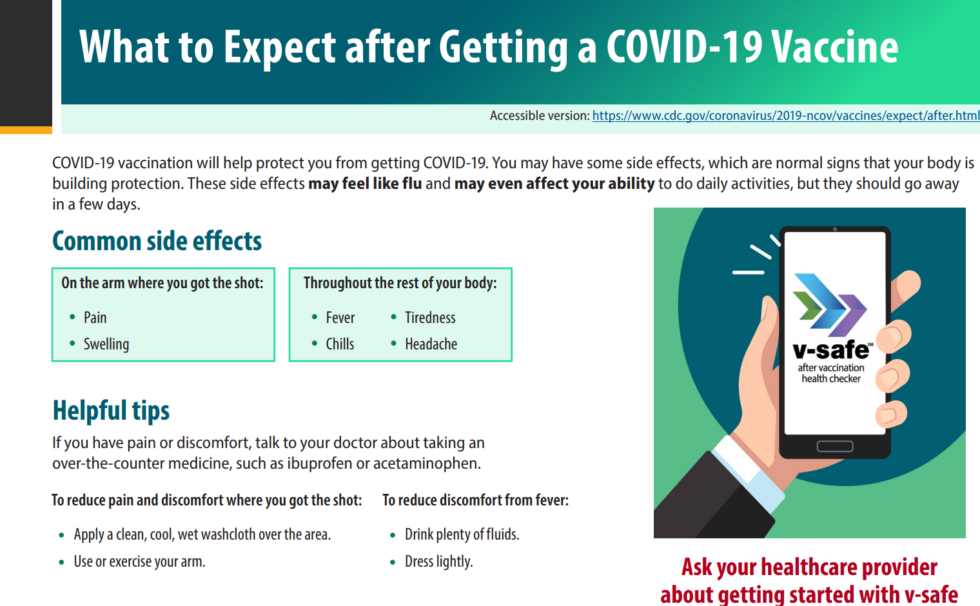
Some people report having mild side effects after flu vaccination. The most common side effects from flu shots are soreness, redness, tenderness or swelling where the shot was given. Low-grade fever, headache and muscle aches also may occur. If these reactions occur, they usually begin soon after vaccination and last 1-2 days.
Side effects from the nasal spray flu vaccine may include: runny nose, wheezing, headache, vomiting, muscle aches, fever, sore throat and cough. If these problems occur, they usually begin soon after vaccination and are mild and short-lived. The most common reactions people have to flu vaccines are considerably less severe than the symptoms caused by actual flu illness.
What about serious reactions to flu vaccine?
Serious allergic reactions to flu vaccines are very rare. If they do occur, it is usually within a few minutes to a few hours after vaccination. While these reactions can be life-threatening, effective treatments are available.
What about people who get a seasonal flu vaccine and still get sick with flu symptoms?
There are several reasons why someone might get flu symptoms even after they have been vaccinated against flu.
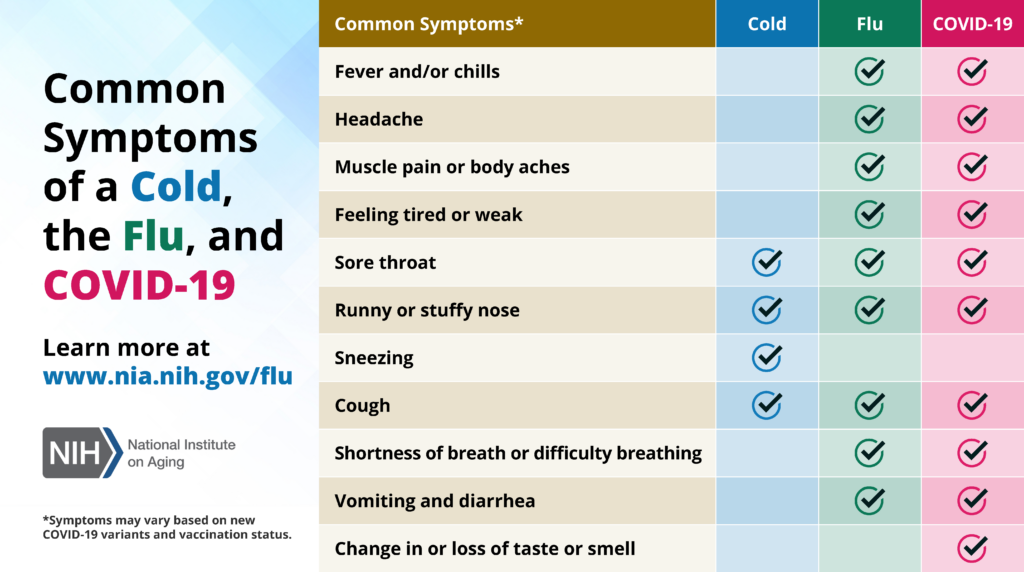
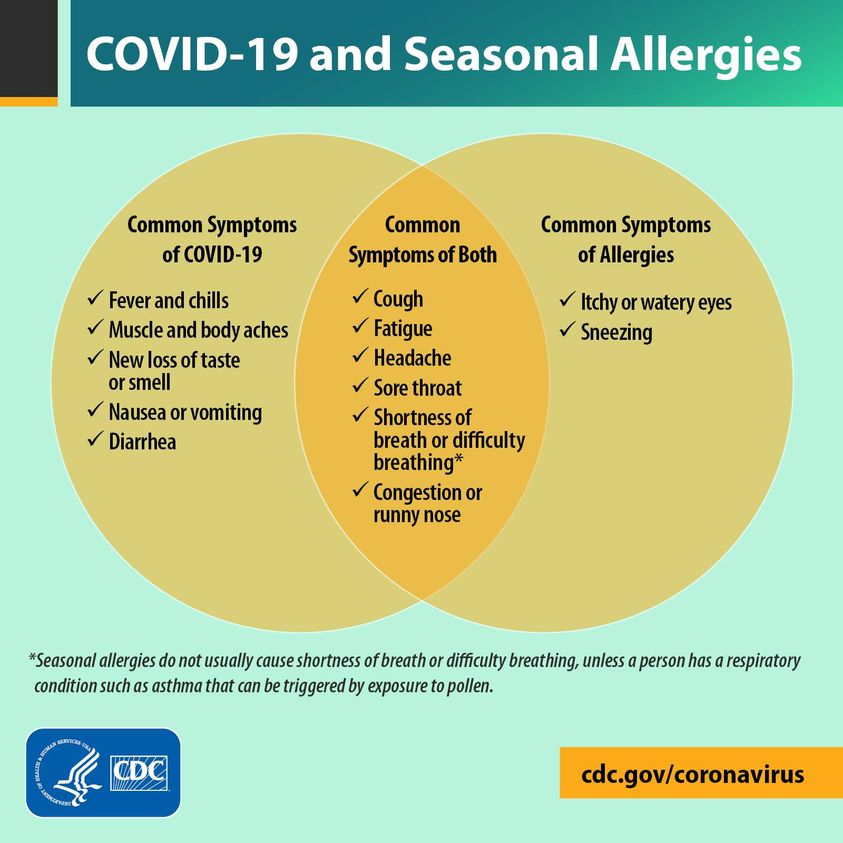
- Someone can get sick with another respiratory virus besides flu such as rhinoviruses or SARS-CoV-2 (the virus that causes COVID-19). Other respiratory viruses can cause symptoms similar to flu, and they can also spread and cause illness during flu season. Flu vaccines only protect against flu and its complications, not other illnesses.
- Someone can be exposed to flu viruses shortly before getting vaccinated or during the two-week period after vaccination that it takes the body to develop immune protection. This exposure may result in a person becoming sick with flu before protection from vaccination takes effect.
- Flu vaccines vary in how well they work, and someone can get vaccinated but still get sick with flu. There are many different flu viruses that spread and cause illness among people, so this can happen if someone is exposed to a flu virus that is very different from the viruses in the flu vaccine. The ability of a flu vaccine to protect a person depends partially on the similarity or “match” between the vaccine viruses chosen to make vaccine and those spreading and causing illness. Even when that happens though, flu vaccination can still reduce severity of illness.
Can vaccinating someone twice provide added immunity?
In adults, studies have not shown a benefit from getting more than one dose of vaccine during the same influenza season, even among elderly persons with weakened immune systems. Except for children getting vaccinated for the first time, only one dose of flu vaccine is recommended each season.
Is it true that getting a flu vaccine can make you more susceptible to other respiratory viruses?
Flu vaccines are not thought to make people more susceptible to other respiratory infections.
A 2012 study that suggested that flu vaccination might make people more susceptible to other respiratory infections. After that study was published, many experts looked into this issue further and conducted additional studies to see if the findings could be replicated. No other studies have found this effect. It’s not clear why this finding was detected in the one study, but the majority of evidence suggests that this is not a common or regular occurrence and that flu vaccination does not, in fact, make people more susceptible to other respiratory infections.
Does a flu vaccination increase your risk of getting COVID-19?
There is no evidence that getting a flu vaccination increases your risk of getting sick from a coronavirus, like the one that causes COVID-19.
You may have heard about a study published in January 2020 that reported an association between flu vaccination and risk of four commonly circulating seasonal coronaviruses, but not the one that causes COVID-19. This report was later found to be incorrect.
The results from that initial study led researchers in Canada to look at their data to see if they could find similar results in their population. The results from this study showed that flu vaccination did not increase risk for these seasonal coronaviruses. The Canadian findings highlighted the protective benefits of flu vaccination.
The Canadian researchers also identified a flaw in the methods of the first study, noting that it violated the part of study design that compares vaccination rates among patients with and without flu (test negative design). This flaw led to the incorrect association between flu vaccination and seasonal coronavirus risk. When these researchers reexamined data from the first study using correct methods, they found that flu vaccination did not increase risk for infection with other respiratory viruses, including seasonal coronaviruses.
Top of Page
MISCONCEPTIONS ABOUT FLU VACCINE EFFECTIVENESS
Influenza (flu) vaccine effectiveness (VE) can vary. The protection provided by a flu vaccine varies from season to season and depends in part on the age and health status of the person getting the vaccine and the similarity or “match” between the viruses in the vaccine and those in circulation. During years when the flu vaccine match is good, it is possible to measure substantial benefits from flu vaccination in terms of preventing flu illness and complications. However, the benefits of flu vaccination will still vary, depending on characteristics of the person being vaccinated (for example, their health and age), what flu viruses are circulating that season and, potentially, which type of flu vaccine was used. More information is available at Vaccine Effectiveness – How well does the Flu Vaccine Work.
Below is a summary of the benefits of flu vaccination and selected scientific studies that support these benefits.
- Flu vaccination can keep you from getting sick with flu.
- Flu vaccine prevents millions of illnesses and flu-related doctor’s visits each year. For example, during 2019-2020, the last flu season prior to the COVID-19 pandemic, flu vaccination prevented an estimated 7.5 million influenza illnesses, 3.7 million influenza-associated medical visits, 105,000 influenza-associated hospitalizations, and 6,300 influenza-associated deaths.
- During seasons when flu vaccine viruses are similar to circulating flu viruses, flu vaccine has been shown to reduce the risk of having to go to the doctor with flu by 40% to 60%.
- Flu vaccination has been shown in several studies to reduce severity of illness in people who get vaccinated but still get sick.
- A 2021 study showed that among adults hospitalized with flu, vaccinated patients had a 26% lower risk of intensive care unit (ICU) admission and a 31% lower risk of death from flu compared with those who were unvaccinated.
- A 2018 study showed that among adults hospitalized with flu, vaccinated patients were 59% less likely to be admitted to the ICU than those who had not been vaccinated. Among adults in the ICU with flu, vaccinated patients on average spent four fewer days in the hospital than those who were not vaccinated.
- Flu vaccination can reduce the risk of flu-associated hospitalization.
- Flu vaccine prevents tens of thousands of hospitalizations each year. For example, during 2019-2020 flu vaccination prevented an estimated 105,000 flu-related hospitalizations.
- A 2018 study showed that from 2012 to 2015, flu vaccination among adults reduced the risk of being admitted to an ICU with flu by 82%.
- A 2017 study found that during 2009-2016, flu vaccines reduced the risk of flu-associated hospitalization among older adults by about 40% on average.
- A 2014 study showed that flu vaccination reduced children’s risk of flu-related pediatric intensive care unit (PICU) admission by 74% during flu seasons from 2010-2012.
- Flu vaccination is an important preventive tool for people with certain chronic health conditions.
- Flu vaccination has been associated with lower rates of some cardiac events among people with heart disease, especially among those who have had a cardiac event in the past year.
- Flu vaccination can reduce the risk of a flu-related worsening of chronic lung disease (for example, chronic obstructive pulmonary disease (COPD) requiring hospitalization).
- Among people with diabetes and chronic lung disease,flu vaccination has been shown in separate studies to be associated with reduced hospitalizations from a worsening of their chronic condition.
- Flu vaccination during pregnancy helps protect pregnant people from flu during and after pregnancy and helps protect their infants from flu in their first few months of life.
- A 2013 study showed that during the 2010–2011 and 2011–2012 flu seasons vaccination reduced the risk of flu-associated acute respiratory infection in pregnant people by about one-half.
- A 2018 study showed that getting a flu shot reduced a pregnant person’s risk of being hospitalized with flu by an average of 40% from 2010-2016.
- A number of studies have shown that in addition to helping to protect pregnant people from flu, a flu vaccine given during pregnancy helps protect the baby from flu for several months after birth, when babies are too young to be vaccinated.
- Flu vaccine can be lifesaving in children.
- A 2022 study showed that flu vaccination reduced children’s risk of severe life-threatening influenza by 75%.
- A 2020 study found that during the 2018-2019 flu season, flu vaccination reduced flu-related hospitalization by 41% and flu-related emergency department visits by half among children (aged 6 months to 17 years old).
- A 2017 study was the first of its kind to show that flu vaccination can significantly reduce children’s risk of dying from flu.
- Getting vaccinated yourself may also protect people around you, including those who are more vulnerable to serious flu illness, like babies and young children, older people, and people with certain chronic health conditions.
Despite the many benefits offered by flu vaccination, only about half of Americans get an annual flu vaccine. During an average flu season, flu can cause millions of illnesses, hundreds of thousands of hospitalizations and tens of thousands of deaths. Many more people could be protected from flu if more people got vaccinated.
*References for the studies listed above can be found at Publications on Influenza Vaccine Benefits.
MISCONCEPTIONS ABOUT THE TIMING OF SEASONAL INFLUENZA VACCINATION
Should I wait to get vaccinated so that my immunity lasts through the end of the season?
How long you are immune or your “duration of immunity” is discussed in the ACIP recommendations. While delaying getting of vaccine until later in the fall may lead to higher levels of immunity during winter months, this should be balanced against possible risks, such as missed opportunities to receive vaccine and difficulties associated with vaccinating a large number of people within a shorter time period.
Is it too late to get vaccinated after Thanksgiving (or the end of November)?
No. Vaccination can still be beneficial as long as flu viruses are circulating. If you have not been vaccinated by Thanksgiving (or the end of November), it can still be protective to get vaccinated in December or later. Flu is unpredictable and seasons can vary. Seasonal flu disease usually peaks between December and March most years, but disease can occur as late as May.
MISCONCEPTIONS ABOUT PHYSICIAN CONSENT FOR VACCINATION
Do pregnant people or people with pre-existing medical conditions need special permission or written consent from their doctor to get a flu vaccine?
No. There is no recommendation for pregnant people or people with pre-existing medical conditions to seek special permission or secure written consent from their doctor for vaccination if they get vaccinated at a worksite clinic, pharmacy or other location outside of their physician’s office. With rare exception, CDC recommends an annual flu vaccine for everyone 6 months of age and older, including pregnant people and people with medical conditions.
A variety of flu vaccines are available (Table 1). Vaccine providers should be aware of the approved age indications of the vaccine they are using and of any contraindications or precautions. Providers also should appropriately screen all people getting vaccinated for allergies to vaccine components or other contraindications. People who have previously had a severe allergic reaction to influenza vaccine or any of its ingredients should generally not be vaccinated.
There are some people who should not get a flu vaccine without first speaking with their doctor. These include:
- People who have a moderate-to-severe illness with or without a fever (they should wait until they recover to get vaccinated), and
- People with a history of Guillain-Barré Syndrome (a severe paralytic illness, also called GBS) that occurred after receiving influenza vaccine and who are not at risk for severe illness from influenza should generally not receive vaccine. Tell your doctor if you ever had Guillain-Barré Syndrome. Your doctor will help you decide whether the vaccine is recommended for you.
Pregnant people or people with pre-existing medical conditions who get vaccinated should get a flu shot.
If a person is vaccinated by someone other than their primary health care provider, the vaccinating provider should ensure that the patient and, if possible, the patient’s medical provider have documentation of vaccination.
For a complete list of people who should not get a flu vaccine before speaking with their doctor, please review the influenza Vaccine Information Statement for the inactivated or recombinant flu vaccine or live, intranasal influenza vaccine.
MISCONCEPTIONS ABOUT “STOMACH FLU”
Is the “stomach flu” really flu?
No. Many people use the term “stomach flu” to describe illnesses with nausea, vomiting or diarrhea. These symptoms can be caused by many different viruses, bacteria or even parasites. While vomiting, diarrhea, and being nauseous or “sick to your stomach” can sometimes be related to flu — more commonly in children than adults — these problems are rarely the main symptoms of influenza. Flu is a respiratory disease and not a stomach or intestinal disease.
To learn more, please visit https://www.cdc.gov/flu/prevent/misconceptions.htm.